As the quest to capture brain waves beyond the sleep lab continues, EEG electrodes will likely soon capture signals from surprising locations (minus today’s globs of gel).
By Sree Roy
The sleep techs I’ve spoken to all say the electroencephalogram (EEG) signal—out of the multitude of physiological recordings gathered during in-lab polysomnography—is the most difficult to capture. “We’re talking about trying to measure voltages that are really super small—in the microvolt range,” says Todd M. Eiken, RPSGT, FAAST, vice president of product development at sensor and electrode maker Dymedix Diagnostics.
Everyday happenings like outside sounds and patient movement can make the signal unintelligible. The contact between EEG electrodes and skin must be pristine. “Otherwise, it’s just going to be noise,” Eiken says.
If brain waves are so difficult to measure in controlled environments such as sleep disorders centers, then they must be near-impossible to measure in real-world settings. Plus EEG alone is not worth much in sleep medicine; movements of the eyes (known more technically as electrooculogram or EOG) and muscles (known as electromyography or EMG) are needed to confirm sleep staging.
Sleep EEG in real-world settings means rethinking the fundamentals of capturing brain waves: The solution is likely not the 10-20 system of wet electrode placement that is gelled onto abraded skin but one of a variety of emerging alternatives—among them, an in-ear design, a “smart skin” dry electrode, and a single-channel EEG with algorithms that account for muscle and eye movements.
“The race to develop the most convenient and accurate home sleep testing based on EEG technology has been going on for quite some time,” says Richard Kaplan, PhD, president at General Sleep Corp, which offers one such solution in its Zmachine Synergy & Zmachine Insight/Insight+ products. “The challenge is to have an EEG system that is easy for the patient to apply without compromising robust clinical data about sleep stages…and all of this needs to happen without intimidating or confusing the patient.”
This is where emerging technologies enter the scene. For instance, sleep EEG technology in development by Zeto Inc, a company that makes a no-prep full-montage EEG headset used by intensive care units (ICU) and epilepsy centers, uses active electrodes instead of the traditional passive ones. “Active electrodes are meant to handle higher impedances,” says Zeto founder and CEO Aswin Gunasekar, MS, MBA, who has a background in electrical and computer engineering. “You don’t have the brain signal traversing a whole long wire to an amplifier.” Instead, pre-amplification is done above the electrode itself. “It’s like a gasoline car versus an electric car; it’s fundamentally different,” Gunasekar says.
While a marketable sleep EEG system is still several years away for the company, Gunasekar says the design Zeto is developing is as “comprehensive as what a sleep lab would do, minus the wires and gluing down electrodes.” It expects to incorporate multiple EEG channels on the head plus an extension box for polysomnograms, as well as accommodate breathing rate and other metrics so sleep specialists can view traditional waveforms.
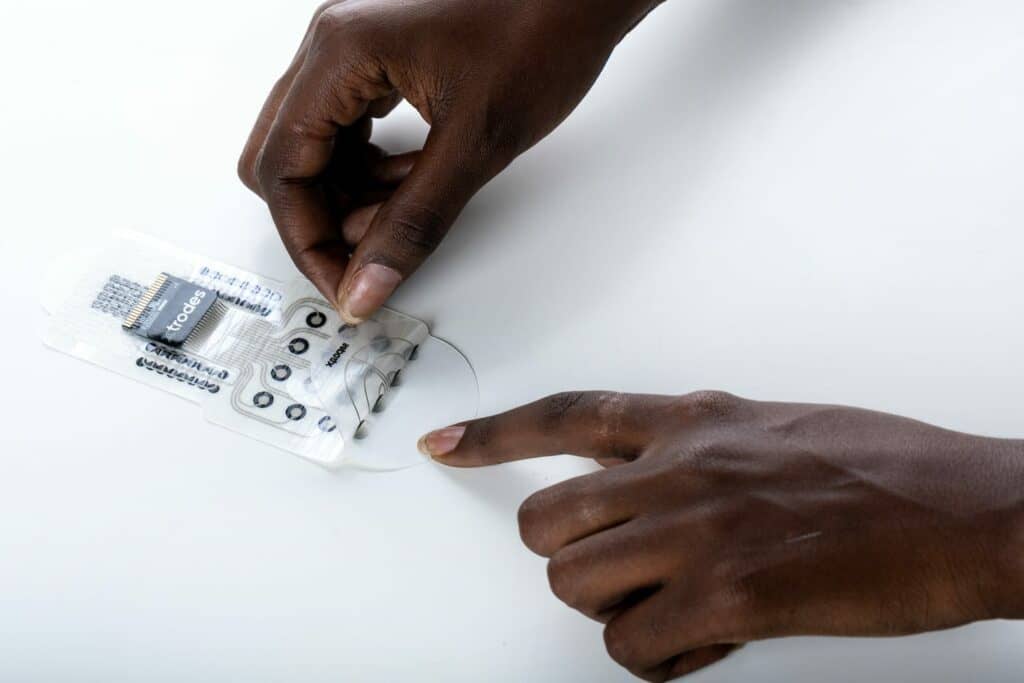
Sleep specialists may also soon see a sleep EEG solution from X-trodes, an electrophysiology company that sells its sticker-like dry electrodes to researchers who collect signals ranging from brain waves to olfactory activations to the heart’s electrical activities. X-trodes is working on US Food and Drug Administration (FDA) approval for clinical applications. “We call it ‘smart skin,’” says Ziv Peremen, PhD, X-trodes CEO. “They are a perfect match to skin with good signal quality, and they maintain their location.”
Partnering with Tel Aviv University in Israel, X-trodes’ solution has shown promise in staging sleep accurately even in challenging situations, such as in people with REM sleep behavior disorder, a neurological sleep disorder characterized by REM sleep without atonia—a symptom that can trick some analyzers into interpreting REM sleep as nonREM. “This is a huge step to show you can actually use this kind of measure in the home environment,” Peremen says.
Home users may readily accept technologies that resemble those they already use. In this vein, an emerging solution by the Center for Ear EEG at Aarhus University in Denmark resembles wired earbuds. Developers, led by the head of the center Preben Kidmose, PhD, embed mushroom-shaped electrodes (designed just for this purpose) into a flexible surface to comfortably fill the curve of human ears, and a wire connects the two earpieces.
Nineteen of 20 wearers in a recent study found the ear-EEG did not negatively impact their sleep, and its automatic sleep scoring has an accuracy close to that achieved by manual scoring of scalp EEG.1 A separate study found ear-EEG automatic sleep scoring estimated total sleep time, sleep onset latency, sleep efficiency, and wake after sleep onset with high accuracy and precision, though REM latency and REM fraction of sleep showed high accuracy but low precision.2
Having an electrode in each ear means horizontal eye movements are captured, says Kidmose, who is also a professor in the department of electrical and computer engineering-biomedical engineering at Aarhus University. “It is not as strong as EOG electrodes, but it’s still clearly there,” he says. Muscle movement too is captured. “Our jaw muscles are attached to the skull all the way around the ear,” he explains.
No Skin Prep, Really?
To facilitate user self-application, many technology makers have opted for dry electrodes.
Researchers have been experimenting with iridium oxide electrodes at the Center for Ear EEG. “From an electro-chemical perspective, it’s not a very good electrode,” Kidmose says. “But it is hydrophilic, which means it attracts humidity. And because the body is wet, after a while hydrophilic electrodes will act more like wet electrodes—so that compensates for the slightly worse electrode characteristics.” They are also trying to make silver/silver chloride electrodes, the type more traditional for clinical applications, more hydrophilic, Kidmose says.
Early on, the Center for Ear EEG would thoroughly clean the ears of its test subjects. But they have since stopped doing any cleaning or other prep. The electrodes work just fine without it. “We thought ear wax would be a problem,” Kidmose says. “But it so happens that ear wax is not a bad thing.” (It helps that ears are relatively hairless compared to the traditional placement areas of EEG electrodes. So far, no research subjects have had their ear hair interfere with reliable signal capture.)

At Zeto, the integrated preamplifiers at the recording sites on its zEEG increase the signal-to-noise ratio such that skin impedance up to 1,000 kOhm will still produce a viable EEG. So the dry electrode headset does not need skin preparations, gels, pastes, or other adhesives. The device, which received FDA clearance in 2018 for prescription use in healthcare facilities and clinical research environments to acquire, transmit, display, and store EEG and optional auxiliary signals, is today primarily used by ICUs and epilepsy centers that “do not have the staff to glue down electrodes,” according to Gunasekar.
General Sleep uses a different tactic. It uses traditional wet chemistry silver/silver chloride EEG sensors with its Zmachine Synergy home sleep testing system, but the sensors are pre-gelled. “They are both easy to apply and highly stable, and the low the skin-to-electrode impedances are achieved automatically over the few minutes following sensor application as the gel penetrates the outer layers of the skin,” Kaplan says. The low mass sensors stick firmly onto the skin to reduce noise from patient movements while also being comfortable during sleep. Skin prep is limited to an alcohol prep wipe and air drying.
Waveforms Versus Algorithms
Sleep specialists are trained to interpret the nuances of polysomnograms (PSG). For example, the alpha waves that differentiate sleep from wake are most prominent in the brain’s occipital region, that is, the back of the head—where there is almost always hair. “If you only rely on the frontal brain, you’re going to be limited in the amount of alpha activity that you’ll see,” Eiken says. So how useful is a self-applied sleep EEG if it doesn’t have the exact waveforms clinicians rely on?
Potentially, quite useful. “We will never be able to be able to compete with a full scalp setup,” says Kidmose of the Center for Ear EEG. “But remember that when a person is in a sleep stage it’s their entire cortex in the sleep stage. While it is true that alpha is more dominant in the occipital section, you will still have sleep spindles from all over the cortex. Yes, there will be sleep spindles that we are missing, but techs are also missing some sleep spindles today—but that’s not the important thing. The important thing is that you see some sleep spindles in N2 sleep, and our device captures that.” Indeed, its agreement with scalp recordings is high. “As long as we get Cohen’s kappa in the high 70s, then we are almost on par with scalp recordings,” he says.
But distinguishing between central- and obstructive-related arousals with ear-EEG will need additional sensors that are still to be developed. “We can identify arousals from the EEG, but the interpretation of the arousals require other sensing methodologies. That is in the early days in our lab to integrate into the earpieces, but it is something we are working on,” Kidmose says. For example, a body microphone that would work similarly to a stethoscope to listen to breathing sounds.
X-trodes “smart skin” uses only below-hairline placements, though external electrodes can be added with gel. “From our experience, many sleep disorders and neurological conditions can be measured with only the prefrontal center,” Peremen says. “We do have an EEG montage (not for sleep) that includes behind-the-ear placements for the temporal and parietal lobes, but we’re not sure that we even need those.” X-trodes can also connect its system to traditional respiratory sensors or to its own sensor and analytics for sleep apnea studies.

As the maker of a single-channel EEG device, General Sleep’s devices push the technological challenge onto its signal processing algorithms. “For example, whereas a human sleep technologist was trained to determine REM sleep using all three of EEG, EOG, and EMG, there are REM detection algorithms that can accomplish this using only a single EEG channel,” Kaplan says. “EEG alone for REM sleep determination is useless without EOG and EMG when a human technologist is visually scoring, but signal processing algorithms can detect things in the EEG signal, both in terms of time domain and spectral features, that are basically invisible to human eyes looking at epochs of EEG data on a screen.”
Other sleep electrode makers say they also get requests for self-applied sleep EEG electrodes. At Cadwell, “We are watching the ongoing discussion on this subject, but we agree that inclusion of EOG and EMG alongside EEG is optimal for determining stages of sleep based on the data that is currently available,” says James Blevins, Cadwell product manager. “I do think that REM sleep behavior disorder is one of the opportunities for a good at-home sleep monitor since the behavioral presentation is not typically every night, and our chances of capturing on an in-lab PSG are generally low.” Blevins adds that frequently part of the question will turn toward reimbursement. “We are closely watching reimbursement, customer demand, and American Academy of Sleep Medicine/Centers for Medicare & Medicaid Services guidelines on type 2 PSG testing,” he says.
Leah Hanson, FASET, FACNS, REEGT/EPT, vice president of global sales and marketing at Rhythmlink International LLC, refers to home-based sleep EEG “as the new frontier of EEG and sleep monitoring. “It’s a powerful direction with great promise,” she says. “Even if a device isn’t meeting every need for every patient, the innovations are what shape the future, which we all should embrace.”
Sleep EEG Goes Beyond Sleep Disorders
In addition to their great promise for sleep medicine, emerging technology for easy at-home sleep EEG has clinical applications well beyond screening and diagnosing sleep disorders.
“Sleep is a gold mine for our health,” says X-trodes’ Peremen. For example, changes to sleep architecture over time could potentially assist in predicting, diagnosing, and monitoring psychiatric and neurodegenerative diseases. Also, sleep is a major contributor to the health of other body systems, such as the cardiovascular system. Long-term sleep EEG monitoring could even assist with preventative health measures. Pereman says, “We have been limited in the use of sleep for a small number of sleep disorders because of the cost and the accessibility of the current tools. But if we have such a simple solution that everyone can do by themselves, we open a new dimension of how we can use our sleep to improve our health and well-being.”
Top photo: The Center for Ear EEG at Aarhus University houses an emerging sleep electrode solution that resembles wired earbuds. Credit: AU Foto
References
1. Mikkelsen KB, Tabar YR, Kappel SL, et al Accurate whole-night sleep monitoring with dry-contact ear-EEG. Sci Rep. 2019 Nov 14;9(1):16824.
2. Kjaer TW, Rank ML, Hemmsen MC, et al. Repeated automatic sleep scoring based on ear-EEG is a valuable alternative to manually scored polysomnography. PLOS Digit Health. 2022 Oct 27;1(10):e0000134.





