
Abnormal nocturnal behaviors can be seen with various conditions including NREM parasomnia, REM behavior disorder, movement disorders, as well as seizures. More recently, it has been noted that frontal lobe seizures tend to occur predominantly at night. However, there is still little understanding about nocturnal frontal lobe epilepsy (NFLE) and it is often misdiagnosed. The case of Mr ZZ illustrates several aspects of the relationships between sleep and epilepsy: the often underestimated frequency of nocturnal seizures, the importance of overnight EEG recording, the pro-convulsant effect of NREM sleep for NFLE, and the interesting association of K-complexes with interictal epileptiform discharges.
CASE REPORT
Mr ZZ is a 37-year-old, right-handed man with intractable epilepsy despite vagal nerve stimulator (VNS) implantation. He has had seizures since the age of 8 years. He described his seizures as “petite attacks,” consisting of glazing into a stare, and rare convulsions during childhood.
He initially reported having these staring spells mostly while awake and during the day. He only recognized rare nocturnal events with similar semiology. His seizure frequency varied from three to four times per week to none for a few weeks. However, he denied any abnormal leg movements. Previous EEG studies showed bi-anterior spike/polyspike and slow wave discharges, more prominent on the left, at times with decreased responsiveness and slurred speech. His antiepileptic medications included levetiracetam 2,000 mg bid, carbamazepine 600 mg bid, and topiramate 300 mg bid.
His birth and development history was unremarkable. His medical history was unremarkable except for intractable epilepsy. There were no epilepsy risk factors other than remote family history of a childhood seizure. He is married and has two children (7 and 16 years old), who were healthy without any seizures. His general examination and complete neurological examination are within normal limits.
MRI of the brain showed findings suggestive of a right frontal lobe cavernous malformation, and left temporal and right frontal developmental venous anomalies.
He denied any sleep problems, and his family, whom he lives with, did not report any nocturnal or unusual events such as motor restlessness, sleepwalking, snoring, or abnormal movements. His usual bedtime was 10:30 pm. He was waking up briefly, around 7 am, to take his antiepileptic medication, following which he slept again until 8:30 am, feeling wide awake and refreshed. He denied any difficulty initiating, maintaining, or reinitiating sleep after rare brief awakenings. He rarely took a nap during the day.
Because of intractable epilepsy, he was evaluated in our Epilepsy Monitoring Unit. Upon admission, he reported having staring seizures at least two to four times a week. However, he was not aware of any frequent nocturnal seizures. He denied having any convulsions for several years.
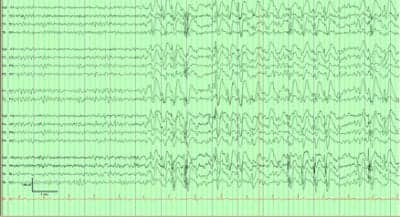
Figure 1. Interictal EEG findings with R>L bi-anteriorly predominant generalized spike/polyspike and wave discharges
After admission to the Epilepsy Monitoring Unit, he had numerous predominantly nocturnal seizures with stereotypical events, consisting of abrupt extension of his legs, followed by bilateral leg bicycling movements with often right arm shaking movement and moaning for several seconds (<20 seconds). Afterward, he appeared to have brief postictal confusion that lasted less than 1 minute. His clinical seizures occurred exclusively out of sleep, eight to 35 times a day, although all of his antiepileptic medications were continued. EEG recording during the stereotypical seizures showed occasional right anterior onset with sharply contoured beta discharges over the right frontal region followed by bilateral spread. His interictal EEG recording showed frequent bursts and runs of high amplitude 2-3 Hz R>L bi-anterior predominant spike/polyspike and wave discharges, up to 20 seconds (Figure 1). Stereotypical nocturnal semiology of bilateral leg bicycling movement and EEG findings of anterior predominant seizure onset were highly suggestive of frontal lobe epilepsy, likely right hemispheric onset (Figure 2).
In order to obtain an ictal SPECT study during the day, his sleep-wake cycle was altered with sleep deprivation until 6 am. With this alteration of sleep cycle, he had typical seizures out of sleep during the late morning until afternoon and hardly had one during the previous night while he was awake. Thus, seizures occurred from sleep regardless of time of day.
Currently, he is undergoing further evaluation with a pending interictal PET scan and is being considered for surgical treatment.
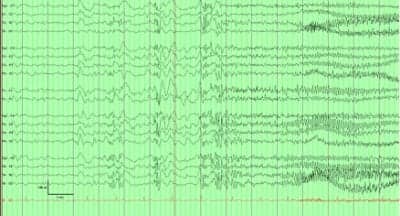
Figure 2. Nocturnal right frontal lobe seizure out of sleep in EEG
DISCUSSION
NFLE is characterized by seizures primarily occurring in sleep, a frontal lobe semiology, and involvement of the mesial and orbitofrontal cortex.1 Electrophysiologic and functional neuroimaging studies support the hypothesis that changes in neuronal excitability associated with sleep are different in each cortical region.
There are distinct neurophysiological changes that characterize stages of sleep. NREM sleep is characterized by cerebral hypersynchrony, mediated by interactions between the brainstem reticular activating system, the thalamus, and the cortex. During NREM sleep, oscillatory or bursting firing of thalamic neurons results in cortical synchronization. REM sleep, on the other hand, is characterized by inhibition of thalamocortical synchronizing mechanisms, a desynchronized EEG pattern, inhibition of spread of epileptiform discharges, and skeletal muscle paralysis.2
It would be therefore expected that pathologic activity in the central nervous system will be different in NREM and REM.3 This would apply to frequency of seizures. Indeed, seizures very rarely occur in REM sleep,2 while NREM sleep is a state when multiple seizures occur, especially among patients with frontal lobe epilepsy.4
In our patient, most of the seizures captured on the Epilepsy Monitoring Unit recording occurred in stage II sleep. Furthermore, when he was sleep-deprived, he had seizures the next morning during stage II sleep. Thus, his seizures appeared to be related to sleep pressure and state of sleep, rather than time of day.

Figure 3. EEG pattern of sleep and K-complexes with questionable embedded discharges
Nocturnal seizures can occur unnoticed, especially in the absence of a bed partner. In our patient, there was a dramatic difference in the number of seizures initially reported by history and the number of events recorded on monitoring. Our patient reported having seizures three to four times per week, yet eight to 35 were recorded on monitoring on the same day. As the seizures occurred from sleep, they were easily missed and the patient was unaware of them. Accurate understanding of seizure frequency is important for optimal therapy. Thus, adequate recording in select cases can establish actual seizure frequency and help treatment.
Patients with epilepsy typically have interictal discharges. These abnormalities are highly specific and help diagnose epilepsy even if seizures are not captured on EEG. Our patient had spike wave activity associated with K-complexes, as presented in Figure 3. Interestingly, NFLE seizures and K-complexes have some common features. For instance, NFLE seizures occur mostly during sleep, primarily in NREM II sleep, which is when K-complexes emerge. Further, K-complexes and NFLE seizures are best seen in the frontal and vertex regions. K-complexes often occur at the initiation of an arousal or a microarousal from sleep. The emergence of an epileptiform discharge embedded in a K-complex could potentially be related to sleep instability created by the CNS pathology.5
Milena Pavlova, MD, is an instructor in neurology at the Brigham and Women’s Hospital/Harvard Medical School, Boston. She is also the medical director at the Faulkner Hospital Sleep Center. Hae W. Shin, MD, Shraddha Srinivasan, MD, and Tracey A. Milligan, MD, are based at Brigham and Women’s Hospital, a teaching affiliate of Harvard Medical School. The authors can be reached at [email protected].
REFERENCES
- Ryvlin P, Rheims S, Risse G. Nocturnal frontal lobe epilepsy. Epilepsia. 2006;47(Suppl 2):83–86.
- Herman ST, Walczak TS, Bazil CW. Distribution of partial seizures during the sleep-wake cycle. Neurology. 2001;56:1453-1459.
- Rossi GF, Colicchio G, Pola P, Roselli R. Sleep and epileptic activity. Epilepsy Res Suppl. 1991;2:23–30.
- Pavlova M, Shea SA, Bromfield EB. Day/night patterns of focal seizures. Epilepsy Behav. 2004;5:44–49.
- Si Y, Liu L, Li Q, et al. Features of the K-complex waves in refractory nocturnal frontal lobe epilepsy. Epilepsy Res. 2010;92:219-225.



