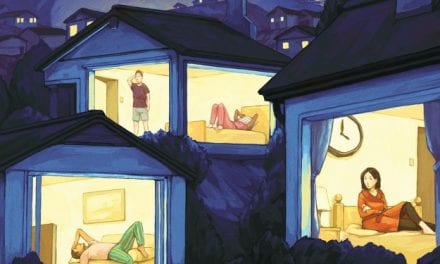
Women, minorities, and people with heart conditions are a few underserved populations that could benefit from home sleep testing.
By April G. Reese
Obstructive sleep apnea, a disorder strongly linked to cardiovascular disease, metabolic disease, and increased mortality, is all too common: Almost one billion people globally have it, according to a 2019 study. The US has one of the highest rates of the disorder in the world, exceeded only by China.1
Underserved populations are especially at risk.2 But studies have found these populations are less likely to be diagnosed and treated for obstructive sleep apnea than the general population. People in these communities are often uninsured, and the cost of traveling to a sleep lab or hospital, having to take time off work, and a lack of awareness of the risks of the disorder means that some of the very people who need treatment the most go undiagnosed.3
Home sleep tests can help close the diagnosis gap, some sleep medicine stakeholders say. In recent years, these tests have improved in design and accuracy. Today’s home devices can collect far more than respiratory effort, airflow, and oximetry; some can now detect brainwaves and leg movements as well, for example. Technological advances can help ensure that people from some underserved populations, such as women, don’t fall through the cracks.
The tests are also becoming easier for patients to use, removing another potential barrier to testing. A 2022 review article notes that wearable devices and artificial intelligence are making these tests easier to administer at home than ever.4 At the same time, public awareness of the importance of quality sleep is on the rise.
Sleep tests conducted in a laboratory remain the gold standard for diagnosing sleep disorders. But in-lab tests come with a number of challenges. “We only have so many labs; we only have so much capacity,” says Carlos Teixeira, clinical affairs manager at Nox Medical, maker of a palm-sized home sleep test for diagnosing sleep apnea. “And there’s a shortage of technicians.”
Even if a patient or their physician can find a lab with available appointments, staying the night at a lab can be impractical, particularly for people with childcare obligations, nighttime work schedules, and/or discomfort staying in a foreign place.3 The nearest sleep lab may be on the other side of the city—or county—and require hours of travel, says Kyle Miko, CRT/CSE, co-founder and chief marketing officer of VirtuOx. “That’s taxing in itself,” he says. An overnight stay also might require taking time off work and finding childcare, Teixeira adds. And even with insurance, a trip to a lab can be costly, particularly for those who are uninsured.
These barriers mean that many of the people most in need of testing and treatment remain unable to get it. “There a lot of studies that show underserved populations, especially Black and Hispanic, are sleep-deprived,” Teixeira says. They may be working two or three jobs while also caring for children and elders.
By contrast, home sleep tests can be delivered to the patient’s doorstep, bypassing the time and expense needed to travel to a lab. For those without insurance, home testing devices are also far cheaper, starting at about $150 as opposed to $1,000 or more for a test in a laboratory.
The tests vary in design. The Nox A1s, for example, is “the exact same device we use for level I we use for level II,” Teixeira says.
ZOLL Itamar makes a home sleep test that uses Peripheral Arterial Tone (PAT), a noninvasive measure of the arterial pulsatile volume changes at the patient’s fingertip. The PAT signal attenuation and accelerated pulse rate has been shown to reflect sympathetic activation, a surrogate for autonomic arousals and micro-arousals found in sleep-disordered breathing.5 Combined with oximetry desaturations or resaturations, the proprietary WatchPAT algorithm classifies the events into the apnea-hypopnea index, respiratory disturbance index, and oxygen desaturation index.
Providers can offer either a reusable device, which is worn overnight and then returned to the provider to upload and review the data, or a disposable device (WatchPAT ONE) that uses a smartphone app to transmit the study data to the cloud. As soon as the study is completed, the clinician can review the automated study results. “Both options provide excellent solutions to support underserved patients and offer a seamless solution,” says Lauren Kinney-Kruse, MS, senior cardiology marketing manager for ZOLL Itamar.
Despite recent advances, home sleep testing is not designed to replace in-lab sleep studies. But home sleep testing has certain advantages to support underserved populations.
“Our goal is not to replace the lab tests,” says Melih Alvo, senior director of commercial marketing at ZOLL Itamar. “There should be in-lab studies.” Kinney-Kruse adds that home sleep tests will hopefully increase the likelihood that at-risk people from underserved populations get the treatment they need.
Improved collaboration between primary care providers and sleep medicine specialists is also crucial to ensure fewer people are left behind. A 2022 study by Vanderbilt University researchers suggested that cultivating such partnerships can increase screening, testing, and treatment among underserved populations. They implemented a specialty sleep clinic at the university’s student-run, free primary care clinic. Patients with sleep apnea symptoms were identified at primary care appointments and screened via a questionnaire. Clinic visits took place over telehealth. Patients then were diagnosed using a home sleep test and, if indicated, prescribed and given a CPAP, with adherence monitored using a cloud-based remote monitoring system.3
Kinney-Kruse, who was not involved in the study, says a goal at ZOLL Itamar “is to increase awareness and increase screening” for sleep apnea. “Home sleep apnea testing offers an opportunity for sleep medicine providers to partner with a number of specialties to increase awareness and promote follow-through for testing, diagnosis, and treatment. We are here to support providers as they work to improve the lives of their patients,” she says.
A lack of awareness of sleep apnea and other sleep disorders in these populations is also contributing to the lack of treatment in underserved populations. For example, many people don’t realize that an undiagnosed sleep disorder is linked to cardiovascular disease, Miko says. “I think we need to do a better job of educating the public about the symptoms and how easy it is to get tested in the comfort of your own home,” he says. “Cardiovascular disease is the biggest killer around the globe. If you want to fix your heart, you’ve got to fix your sleep.”
April G. Reese is a science journalist, editor, and audio producer.
References
1. Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug;7(8):687-98.
2. Dong L, Dubowitz T, Haas A, et al. Prevalence and correlates of obstructive sleep apnea in urban-dwelling, low-income, predominantly African-American women. Sleep Med. 2020 Sep;73:187-95.
3. Henry O, Brito A, Lloyd MC, et al. A model for sleep apnea management in underserved patient populations. J Prim Care Community Health. 2022 Jan-Dec;13:21501319211068969.
4. Korkalainen H, Nikkonen S, Kainulainen S, et al. Self-applied home sleep recordings: the future of sleep medicine. Sleep Med Clin. 2021 Dec;16(4):545-56.
5. Yalamanchali S, Farajian V, Hamilton C, et al. Diagnosis of obstructive sleep apnea by peripheral arterial tonometry: meta-analysis. JAMA Otolaryngol Head Neck Surg. 2013;139(12):1343-50.
Illustration 29498067 © Sibgat | Dreamstime.com