A patient’s perspective of the obstacles in managing OSA with oral appliance therapy and surgery.
The long-term management of patients diagnosed with sleep-disordered breathing (SDB) presents many challenges for both the patients and those entrusted with their care. To date, the treatment algorithm has been diagnosis via polysomnography and initial therapy utilizing some form of positive airway pressure therapy in combination with various respiratory interfaces. One has only to look at the number and types of machines, masks, nasal pillows, straps, and headgear to appreciate the fact that this is by no means a one-size-fits-all world or solution. We have a plethora of mechanical, surgical, and behavioral treatment modalities for SDB—the challenge is which one, or combination thereof, and in what order do we apply them?
The following case study is one patient’s tale of his journey along the treatment pathway. The patient’s account is from an appeal he had written to his insurance carrier, which had denied coverage for a new device, replacing the one that had served him for nearly 7 years. It is my hope that this case, as told through the patient’s eyes, will help lead to an appreciation not only of the medical, clinical, and treatment challenges a patient faces, but also the economic and insurance battles that are fought in order to obtain treatment.
| Patient History and Data |
 |
Dear Madam/Sir:
I am in receipt of your March 25, 2008, Predetermination of Benefits Notice of Adverse Determination and I am sending you this letter within sixty (60) days in accordance with your internal appeal/review process.
Based upon your letter, you have made the claim that the custom dental orthotic I have requested is not demonstrated through prevailing peer-reviewed medical literature to be safe and effective in treating my very clearly documented case of sleep apnea, and on that basis you have denied my request for approval of payment for a new device. With all due respect, the decision of your company is flawed, inconsistent with your prior handling of my condition and extremely arbitrary. I am demanding that your decision be reversed and my claim approved immediately.
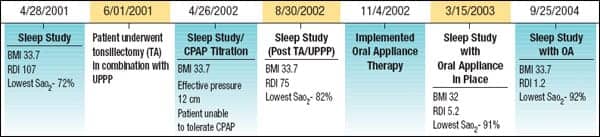
I became very ill and was diagnosed with a severe case of sleep apnea through a sleep study conducted on April 28, 2001; based upon this study, you approved my June 12, 2001, tonsillectomy and UPPP. According to the sleep study, a scientifically objective study, I had 107 breathing disturbances an hour (the current standard allows a normal person to have 5 disturbances and classifies a person with 30 or more disturbances an hour as having severe sleep apnea) and I had some pauses in breathing lasting up to 50 seconds and my oxygen saturations dropped as low as 72%. As a result of my condition, I suffered from headaches constantly, I was exhausted and unable to stay awake for a full day, I was unable to concentrate, read, or work, and the condition also affected my ability to drive. Without any exaggeration, I can tell you that my life was falling apart. I also experienced sweating and the need to get up numerous times a night to urinate (whenever I slept), which I was later advised by one of my doctors was the result of oxygen deprivation caused by my apnea, which could have caused a heart attack or a stroke.
After my first surgery was performed, the number of respiratory disturbances during sleep fell from 107 to 75, still more than twice the classification for severe apnea (30). Please see the enclosed 8/30/02 sleep study. I was horrified after enduring such a painful surgical procedure to learn that I was still so sick. It was decided that since I was no longer an appropriate candidate for CPAP due to the anatomical changes resulting from my UPPP surgery (the air kept blowing out my mouth and the headgear caused pain in my jaw joints), I consulted with Dr Don Pantino for evaluation as a candidate for a custom dental orthotic—which ultimately was my salvation.
I received my dental orthotic in the beginning of November in 2002. By my next sleep study on March 15, 2003 [a copy of which is enclosed], my respiratory disturbance index fell to 5.2; my lowest saturation was 91%! My surgeon advised me on a follow-up visit that he never expected in his wildest dreams that my apnea would or could ever be improved to that degree. The dental device gave me results which were nothing short of a MIRACLE. The enclosed sleep study from September 25, 2004, documented that when using the dental device I had no apnea with a score of only 1.2 disturbances. All of the subsequent sleep studies conducted with the use of the dental device yielded similar results—far from the 75 disturbance index I was experiencing following my initial surgery and before using the dental orthotic. I concede that I am not well versed in the prevailing peer-reviewed medical literature concerning the use of custom dental orthotics for the treatment of sleep apnea; however, my medical records clearly demonstrate that the device has been extremely effective at treating my illness. The person who issued the denial to my request for another dental orthotic could not possibly have reviewed my actual medical records or he would never have issued a denial of the request for another dental device. Based upon my success with the dental orthotic fashioned by Dr. Pantino, I am a textbook example of the device’s success.
Your recent denial is entirely inconsistent with your prior approval of my request for a dental orthotic some six and a half years ago. How is it that the device was acceptable then, but is no longer considered to be safe and effective now and despite my phenomenal sleep study results?
It was determined approximately six weeks ago that my original dental orthotic had reached the end of its effective life (having served me for six and a half years) at which time the request was made for approval of another device. I am now experiencing headaches, exhaustion, difficulties concentrating and staying awake the entire day, and the condition has again affected my ability to drive safely regardless of the amount of sleep that I get. The return of my sleep apnea in the absence of a proper dental orthotic has severely affected my health, my well-being, and my ability to work. I am putting you on notice that I will hold you liable for any medical conditions that I suffer (heart attack/stroke) or for any accidents or injuries that I suffer due to your arbitrary decision to withhold from me clinically proven treatment for my documented case of severe sleep apnea. I will fight this denial like I am fighting for my life, because I am!
DISCUSSION
You will be happy to know that the patient prevailed in getting the denial overturned; more importantly, he is effectively treated with a new appliance. Had the patient not been so persistent, well educated, and versed about his condition, I doubt that he would have won his appeal. Second, had he not had the uvulopalatopharyngoplasty (UPPP), I doubt that he would have had as effective an outcome.
As demonstrated by this case, oral appliance therapy (OAT) can be used in combination with other therapies; OAT in conjunction with UPPP is highly successful.1 Additionally, when positive airway pressure is used in combination with mandibular advancement therapy, the pressure requirement can be reduced on average by 50%, helping to increase CPAP compliance and success.2
Regarding the scientific literature surrounding OAT, insurance companies, health care providers, and the public should be aware of the 2005 American Academy of Sleep Medicine update of its position paper on the use of oral appliance therapy for the treatment of obstructive sleep apnea,3 which addresses the scientific, clinical, and academic concerns of OAT. (A copy can be viewed on the American Academy of Dental Sleep Medicine’s Web site, www.aadsm.org.) This update is significant in that OAT is no longer considered a last resort therapy. The literature clearly demonstrates that OAT is, and continues to be, an effective therapy in the management of SDB. The new guideline’s most important recommendation is that OAT is an appropriate first-line therapy for snoring and mild and moderate SDB, and is appropriate for severe cases that are unsuccessful with other therapies, mainly positive airway pressure. It is important to note that it was not just the AASM position paper that had come to these conclusions; work had been done around the world by others with similar findings and recommendations.4-7
It is generally agreed that OSA is multifactorial in origin and is best approached in a multidisciplinary fashion. I believe that whatever therapeutic approach is taken, in the end, treatment success may best be determined by the patient’s needs, desires, and participation in the process.
Don A. Pantino, DDS, DABDSM, is a past president of the American Academy of Dental Sleep Medicine, serves as treasurer of the American Board of Dental Sleep Medicine, and is chair of the dental school curriculum committee of the AADSM. He is an associate clinical instructor at SUNY Stony Brook School of Dental Medicine and maintains a private practice in Long Island, NY, with a concentration on the treatment of sleep-disordered breathing.
REFERENCES
- Millman RP, Rosenberg CL, Carlisle CC, Kramer NR, Kahn DM, Bonitati AE. The efficacy of oral appliances in the treatment of persistent OSA after uvulopalatopharyngoplasty. Chest. 1998;113:992-96.
- Denbar MB. A case study involving the combination treatment of an oral appliance and auto-titrating CPAP unit. Sleep Breath. 2002;6(3):125-8.
- Kushida CA, Morgenthaler TI, Littner MR, et al. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: an update for 2005. Sleep. 2006;29:240-3.
- Hoekema A, Stegenga B, DeBont LG, Efficacy and co-morbidity of oral appliances in the treatment of obstructive sleep apnea-hypopnea: a systematic review. Crit Rev Oral Biol Med. 2004;15(3):137-55.
- Lim J, Lasserson T, Fleetham J, Wright J. Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD004435.
- Cohen R. Limited evidence supports use of oral appliances in obstructive sleep apnea. Evid Based Dent. 2004;5(3):76.
- Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29:244-62.




