For drug-induced sleep endoscopy to determine sleep apnea therapy candidacy, the first 10+ minutes may not be representative of airway collapse.
By Alyx Arnett
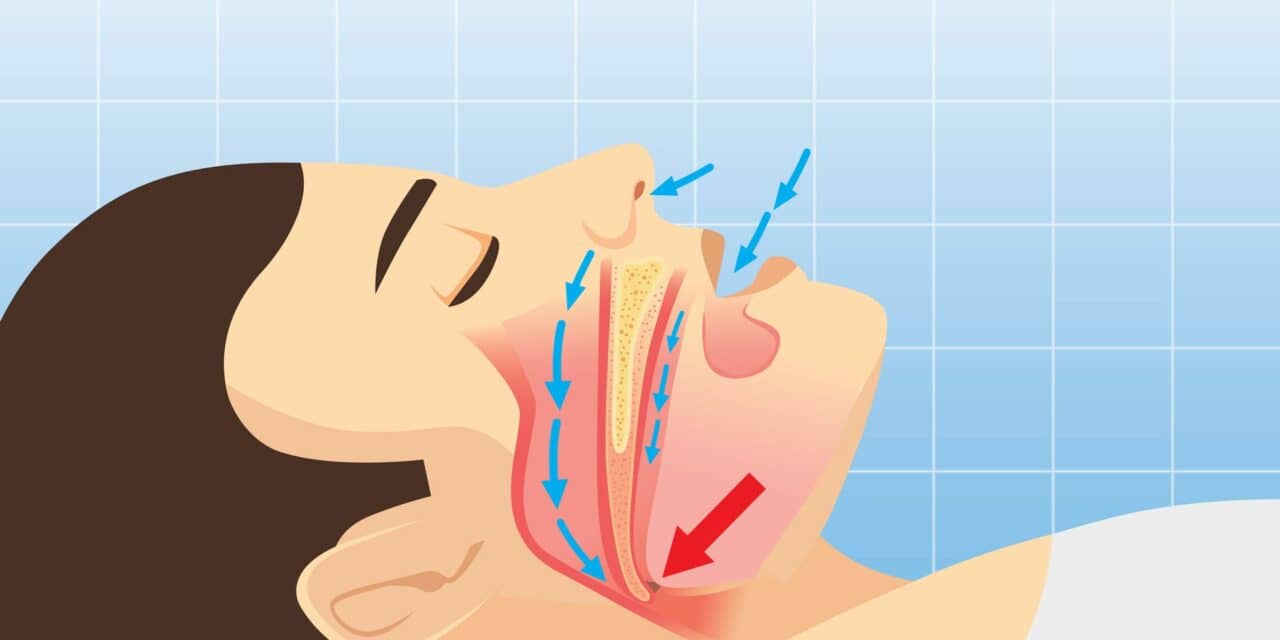
Nearly half of sleep apnea patients undergoing drug-induced sleep endoscopy (DISE)—which assesses the upper airway of patients while under sedation to determine whether a patient is a candidate for a specific therapy, such as an Inspire Medical neurostimulator—exhibit central and mixed apnea events in the early phases of the procedure, even if they were previously diagnosed with only obstructive events during a routine sleep study, according to a study presented at the 2023 American Academy of Otolaryngology–Head and Neck Surgery annual meeting.
This finding has implications for the minimum duration needed for DISE procedures for airway analysis.
The study was prompted after sleep surgeons at the University of Pennsylvania noticed that sentinel central and/or mixed events (SCents) seemed somewhat common during the initial period of DISE. The team’s platform included the simultaneous collection of respiratory airflow and effort measurements, airway collapsibility, and videoendoscopy, allowing them to better categorize the upper airway during DISE.
The study involved 104 patients who underwent DISE with propofol sedation. While investigators expected to see some SCents, they were surprised by the prevalence: Almost 50% of patients had at least one.
Researchers also saw that most SCents eventually transitioned to obstructive events. But that transition took about 12 minutes—which is often longer than the average duration of a DISE exam, according to study co-author Raj C. C. Dedhia, MD, MSCR, associate professor of otorhinolaryngology and medicine at the Division of Sleep Surgery, Penn Otorhinolaryngology.
Dedhia says the team was also surprised by the high frequency of different VOTE scores (velum, oropharynx, tongue base, and epiglottis) between SCents and obstructive events (63%). There was a higher tendency for SCents to have more complete tongue base collapse compared to no or partial collapse and to transition from anterior-posterior velum to concentric velum collapse during the obstructive event. According to Dedhia, this could potentially alter sleep apnea neurostimulator candidacy.
“We want providers who offer DISE and PAP alternatives to be aware of the prevalence and timing of SCents and to be mindful of clinical signs of effort (eg, monitor chest and abdomen) during DISE in the absence of respiratory effort belts (ideal method),” says Dedhia. “They may also want to consider lengthening their minimum DISE duration to 10 minutes to ensure that the majority of SCents have passed. If they see SCents, they should delay any VOTE scoring until patients transition to obstructive events.”
Based on the findings, study co-author Alan R. Schwartz, MD, adjunct professor and part-time faculty at the University of Pennsylvania, says that in addition to inspecting the pharyngeal airway and characterizing the site(s) and patterns of collapse, the patient’s breathing pattern should also be noted during DISE.
Central sleep apnea and Cheyne-Stokes respiration are frequently associated with some degree of pharyngeal collapse during central apneic episodes, he adds. “Detecting obstruction is only half the battle. The DISE examiner should also be sure that pharyngeal obstruction is playing a primary role in the pathogenesis of sleep apnea rather than simply resulting from the loss of drive to upper airway muscles during central events,” says Schwartz.
For patients in the study whose sleep disorder was found to be primarily central in nature, “we recommended that therapy be redirected to address the central rather than obstructive sleep apnea in these patients,” says Schwartz.
David Kent, MD, an associate professor in the department of otolaryngology–head and neck surgery and director of sleep surgery at Vanderbilt University Medical Center, who was not involved in this research, says the study adds to a small but growing body of evidence that DISE findings can vary between exams, reviewers, and even over time during the same exam.
Most noteworthy to him were the frequency of central apneas and the duration required to transition to obstructive pathology. “I wonder if they are linked to the rate at which propofol is delivered and the speed at which increases in ventilatory drive build,” Kent says. “There’s a rich body of research questions to ask surrounding these findings.”
Regarding the potential impact on the timing and protocol of DISE, Kent says it is too early to draw clinical conclusions but notes that the findings deserve consideration by sleep surgeons. If further research confirms that changes in examination correlate with surgical outcomes, it would be necessary to modify exam parameters, says Kent.
Asim Roy, MD, medical director of the Ohio Sleep Medicine Institute and a prescriber of Inspire therapy, says he was not surprised by the prevalence of central events during the onset of propofol. He suggests the clinical implications might relate to the degree of sedation.
Dedhia notes that the propofol dosing technique was not standardized across all patients, “which in theory could account for more SCents if patients were more sedated.” He says repeating the study with a standardized propofol approach would further bolster the data.
Reference
Rodin JG, Parekh MH, Cai Y, et al. Prevalence of sentinel central events during drug-induced sleep endoscopy. Presented at AAO/HNSF 2023. Best of Scientific Orals 2. 2023 Oct 1.
Illustration 64509943 © Suriya Siritam | Dreamstime.com