Insomnia Secondary to Obstructive Sleep Apnea

Psychophysiological and pharmacologically mediated forms of insomnia are extremely prevalent, affecting up to 15% of the adult population.1,2 It is important to eliminate obstructive sleep apnea (OSA) as a cause of insomnia prior to instituting pharmacological and/or behavioral treatments. The former can be hazardous in a patient with OSA, as arousal mechanisms during apneas are apt to be blunted by some pharmacological agents. Behavioral modification (such as learning relaxation techniques), while helpful in a patient with insomnia due to psychological reasons, will be of little or no benefit in a patient with OSA.
Patient History
A 36-year-old white male who weighed 86 kg and was 178 cm tall presented to the Sleep Apnea Center, Staten Island University Hospital, Staten Island, New York, complaining of his inability to fall asleep and maintain sleep. Further questioning and discussion with the patient clarified that he perceived that he could not fall asleep for an hour or more after retiring and felt that he was awake for the duration of that period. He remembered looking at the clock every hour and noting the time. He reported multiple awakenings during the night, some lasting half an hour or more. The patient would retire to sleep feeling very tired. He usually tried to relax for about an hour in a dimly lit room prior to retiring, hoping that this practice would help him sleep. He had cut his caffeine consumption to one cup of coffee per day, which was consumed in the morning.
Upon physical examination, it was noted that the patient had narrow pharyngeal pillars, a moderately enlarged tongue, and a moderate retrognathia. Medical history included moderate hypertension under good control with an angiotensin-converting enzyme inhibitor. He had a Mallampati score of IV.
Differential Diagnosis
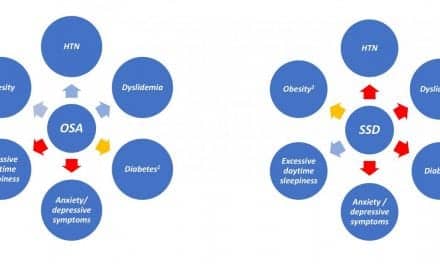
This patient presented with classic signs of sleep-onset insomnia (the inability to fall asleep), but described several factors that broadened the differential diagnosis; these included signs and symptoms suggestive of OSA. The patient complained of excessive daytime somnolence. Patients with classic psychophysiological insomnia, however, are usually overactivated, and they rarely complain of daytime sleepiness. They focus more on being unable to sleep than on the complications of this problem. With the exception of sleep-onset insomnia, this patient’s complaints and physical findings were overwhelmingly suggestive of OSA. They included:
- daytime and early-evening somnolence;
- a crowded posterior oropharynx;
- loud snoring; and
- a moderate degree of retrognathia.
The insomnia in this patient could also have been secondary to abrupt arousals from OSA, coupled with his inability to determine that he was actually falling asleep multiple times prior to entering a continuous sleep period later in the night.
This case also demonstrates psychophysiological insomnia, which usually develops out of frustration over the fact that insomnia is even occurring. This causes the patient to become more stimulated in the morning. Once asleep, he is a loud snorer, about which his wife has complained. The patient is tired and irritable in the morning and has noted that he experiences drowsiness during the day.
Polysomnography
The patient was scheduled for all-night polysomnographic testing with a possible split-night protocol for evaluating OSA. The first part of the night had a total recording time of 149.3 minutes, and total sleep time was 97.5 minutes. The overall sleep efficiency was reduced, at 65.3%. There were six awakenings and 21 stage shifts. Sleep latency was 35.6 minutes.
Latency to rapid–eye-movement (REM) sleep after the onset of sleep was 84.5 minutes. The patient’s reduced sleep efficiency reflects an element of insomnia.
| Differential diagnosis in sleeplessness.
Possible Diagnoses: Testing: |
Of sleep time, 14.9% was spent in stage I, 71.8% in stage II, and 13.3% in REM sleep. There was no stage III or IV sleep. Respiratory data indicated the presence of 88 obstructive apneas with a mean duration of 27.7 seconds and a maximum duration of 52 seconds. There were 38 hypopneas with a mean duration of 17.8 seconds and a maximum duration of 31.2 seconds. The combined apnea/hypopnea index was 77.5 events per hour. The patient was noted to have multiple sleep-onset respiratory events that resulted in prolonged arousals from sleep.
Continuous pulse oximetry revealed that the patient spent 90.5% of the time while asleep at an oxygen saturation (Spo2) of 90% to 100%, 5.2% of the time at an Spo2 of 80% to 90%, and 1.1% of the time at an Spo2 of 70% to 80%. There were no significant leg movements suggestive of periodic limb movement syndrome, and no significant cardiac dysrhythmias were present.
Therapeutic Measures
According to protocol, beginning at 1:27 am, nasal continuous positive airway pressure (CPAP) was initiated at a starting pressure of 4 cm H2O. In response to continued sleep-disordered breathing, CPAP was gradually increased to a maximum level of 12 cm H2O. At this pressure setting, the patient had complete resolution of his sleep-disordered breathing. He maintained sleep and had no further spontaneous awakenings during the time he was on CPAP, which was for the remainder of the night. In the morning, the patient commented that he had slept better than usual.
Discussion
The differential diagnosis of insomnia can consider not only OSA, but a multitude of other diseases and disorders (including pain, anxiety, stress, and depression), as well as the symptoms of many medical conditions such as hyperthyroidism or Cushing disease. Periodic limb movement syndrome may also produce arousals preventing the normal onset of sleep. In addition, some foods and beverages, as well as many prescription and over-the-counter medications, can be responsible for sleeplessness.
Thomas M. Kilkenny, DO, FAASM, is medical director, and Steve Grenard, RRT, is clinical coordinator, both at the Sleep Apnea Center, Staten Island University Hospital, Staten Island, NY.
References
1. Rosekind MR. The epidemiology and occurrence of insomnia. J Clin Psychiatry. 1992;53:4-6.
2. Aldrich MS. Cardinal manifestations of sleep disorders. In: Kryger MH, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. 2nd ed. Philadelphia: WB Saunders; 1994:418-425.