While CPAP continues to be the gold standard for treatment of sleep apnea, oral appliances that thrust the jaw forward during sleep are becoming more popular as a treatment for sleep apnea. A new study in CHEST demonstrates that mandibular movements monitoring can be used to assess the efficacy of these oral appliances.
Mandibular movements during sleep are accurate reporters for increased respiratory effort and microarousals found in people with sleep apnea, the study authors report. In this sleep study, 56 patients with obstructive sleep apnea (OSA) were fitted with a custom mandibular advancement splint and had their midsagittal mandibular movement tracked. Patients were evaluated at the end of the titration procedure. During the titration procedure different degrees of advancement are trialed up and down to find the single best amount to control apnea events for that patient.
“The novelty of the study related to tracking sleep [mandibular movements] in order to assess oral appliance therapy effectiveness,” says lead investigator Jean-Benoit Martinot, MD, Sleep Laboratory, CHU UCL Namur Site Sainte-Elisabeth, Namur, Belgium, in a release. “Our study suggested for the first time that [mandibular movements] monitoring represents a powerful tool for assessing the efficacy of OAT [oral appliance therapy] treatment.”
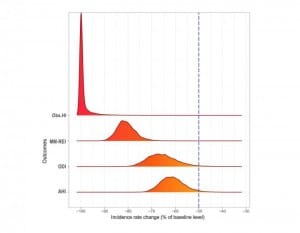
Investigators found that by the end of titration, all indications of OSA decreased compared with baseline. Overall, patients showed a reduction of vertical respiratory mandibular movements and sleep respiratory effort, as well as a dramatic decrease in obstructive hypopnea. Scores from the apnea-hypopnea index and oxygen desaturation index also dropped.
“Using [mandibular movements] measurements in the oral appliance titration procedure has the potential to optimize the benefit/risk ratio of oral appliances,” says Martinot. “There is a high interindividual variability in response to the oral appliances, and it is difficult to predict the range of responses without proper measurement.”
Researchers also found that mandibular movements monitoring helped to reveal the presence of central apneas. They found in a subgroup of subjects a decrease in respiratory effort, but no improvement or an increase in sharp and sudden mandibular movements of high amplitude, which indicates persistent sleep fragmentation. This is highly suggestive of emergent central apneas and may shed light on a possible predictor for poor response to oral appliance therapy.
Mandibular movements monitoring could potentially represent a cost-effective and easy-to-implement tool for sleep clinics to use when titrating oral appliances, the authors say. Mandibular movements “monitoring during sleep is practical and informative for measuring indices of residual respiratory events when OSA is treated by oral appliances,” Martinot says. “Given the growing use of this treatment as the primary alternative to CPAP, these data are relevant for sleep clinicians.”