Reviewing and responding to data collected on PAP therapy patients is necessary to ensure the best therapy at the most reasonable costs.
With the rapid growth of sleep medicine comes the burden of scientific evidence of the value, application, and improved outcomes of new sleep-related devices and systems. Since any rapid increase in health care costs causes payors to evaluate whether the expense is legitimate and appropriate, sleep medicine is, and will continue to be, under the scrutiny of payors. Reviewing and responding to data collected on PAP therapy patients is necessary to ensure the best therapy at the most reasonable costs. The challenge: gathering the data.
FOLLOW-UP SERVICES
Payors are continually focusing on cost of care, challenging providers to monitor effectiveness of products and services. A follow-up service provided by an outside company may allow for more efficient assessment of patients’ therapy and the creation of a database large enough to analyze and respond to effectiveness of products and services. These companies offer services for the follow-up of PAP therapy patients, allowing the provider to utilize a specific company to monitor their patients and recommend follow-up and intervention. This service is justified by the timely renewal of reimbursed supplies, but it also provides another benefit—a large source of patient and product information. Utilizing these services to document and justify the clinical benefits of home PAP therapy will create a scientific foundation to justify products and services in the future. Without this type of evidence, sleep medicine will be as vulnerable as oxygen therapy in the home, which continues to be impacted with reduced reimbursement and the resulting reduction in necessary services.
Contract follow-up services offer their programs to a number of providers, creating a large pool of patient contacts. The quantity of patients and number of calls allow the contract services staff to be very efficient at the phone contacts. The consistent script that is followed allows for a standardization of information that is collected. Subjective data may not be as accurate as objective means of data collection, but it is cost-effective and can provide data on trends.
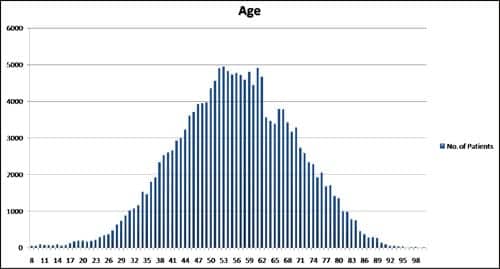 |
| AGE: Data revealed that the highest number of patients receiving PAP therapy follow-up were between the ages of 50 and 62. Further scientific analysis of such data could help solidify studies that have examined incidence of OSA among different age groups. Further analysis also could point to patient populations that are typically not suspect OSA patients. |
Presently, follow-up services are not focused on clinical research since there has been little demand from their customers. Furthermore, most researchers are not aware of the volume of data that is available. This data can be patient neutralized to comply with HIPAA requirements and then the raw numbers can be analyzed and compared. The sheer numbers that are available far exceed the number of patients routinely included in scientific publications, so the possibility of obtaining a better understanding of issues and trends in PAP therapy is a valuable potential of this data.
Once it is analyzed, conclusions can be drawn on trends and issues that may be impacting effective PAP therapy. Research programs also can be established to determine if a change in direction of current practice will impact effectiveness of therapy and outcomes. New protocols and approaches to therapy can be developed based on evidence from a large group of monitored patients. To provide a meaningful impact, this data must be thoroughly and scientifically analyzed, reviewed, and published. Furthermore, without the evidence and the measured outcomes, payors may change reimbursement arbitrarily and impact patient care.
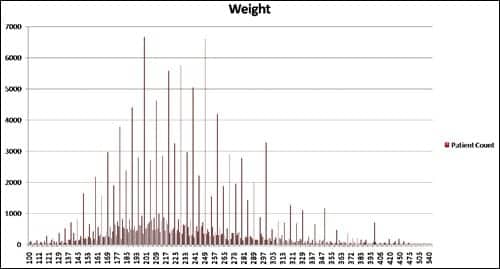 |
| WEIGHT: Sleep-disordered breathing is often associated with an overweight patient. the statistics indicate that while most of the patients in this large database appear to be overweight, there is a wide distribution of patients in different weight ranges. Access to this large source of patient information also may provide opportunities to investigate the relationship of weight to other factors such as disease incidence. |
A GLIMPSE INTO THE DATA
The purpose of this data analysis is to raise awareness of the potential of accessing large databases of patients on PAP therapy. PAP therapy is growing at an amazing pace, and new products and procedures are being utilized with limited review or evaluation of what products or procedures produce the best clinical outcomes as efficiently as possible. The data provided here is not intended to be a scientific assessment with strong evidence to formulate clinical guidelines. The data is provided to stimulate the possibility of looking at larger sources of information to identify, track, and trend PAP therapy in the home.
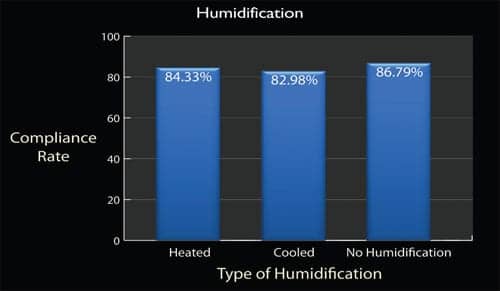 |
| HUMIDIFICATION: Information obtained from patient files indicates that humidification does not appear to have a significant impact on treatment compliance. Compliance from this distribution of patients showed that the humidifiers used did not have a significant impact on their compliance with therapy. In order to effectively cross analyze compliance data from different follow-up services, a standard definition of compliance would need to be set among these services. A standard definition of adherence, such as the definition set forth by CMS for continued coverage of PAP therapy, would be appropriate. |
A national provider of sleep management services shared information on a large patient segment. No specific patient information was shared and all patient privacy was maintained. Files from 167,940 patients were provided for review. Significance of the data was reviewed with trends and observations analyzed to determine if devices or service improved therapy and outcomes.
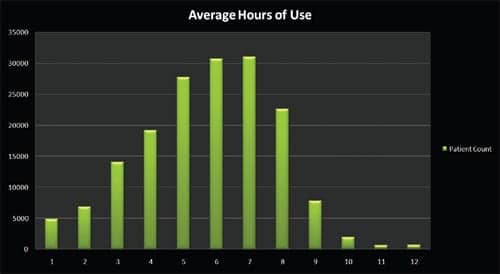 |
| HOURS OF USE: Files indicated that compliance among the 167,940 patients was very good. Was it due to the follow-up? What were the steps taken for patients under 4 hours? Further analyses of such data may provide valuable information for clinicians and providers and help to establish a more comprehensive standard of care with protocols or procedures that ensure adequate use of the technology. |
THIRD-PARTY FOLLOW-UP SERVICE
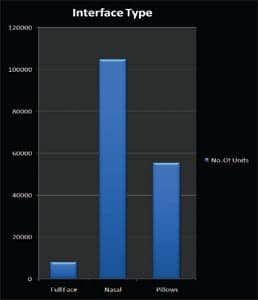 |
| INTERFACE: For this set of data that was reviewed, it appears that nasal interfaces are used more often. |
The provider of this third-party phone follow-up service determined their own sequence of calls, the script used to interview patients, and the training of their staff. Other services may follow a different process, and there will need to be standardization in the future if the data collection grows to be a significant and important source for clinical trend analysis. This service calls patients after 5 days of initiation of PAP therapy and then every 30 days for 3 months, and proceeds with 90-day follow-up intervals for the remaining duration of therapy. The staff asks basic questions related to the patients’ sleep hygiene and basic physical assessments that are easily provided.
Communication with the patient helps to reinforce instructions, provides simple solutions that may be overlooked by the provider, and helps the patient to comply with therapy. Having one source of contact with a large population of therapy patients provides consistency with the follow-up and the ability to establish a large database of information for assessment. The phone follow-up currently does not ensure accurate or objective data, and the patient may be providing information that is not accurate. The reality of providing PAP therapy in a home environment will always allow the possibility that a patient will not be monitored as objectively as in a hospital.
SUMMARY AND CONCLUSION
Sleep medicine is responding to a growing need for diagnostic services and effective PAP therapy. Technology, techniques, and processes are changing at a rapid pace, and both patients and clinicians are attempting to adapt to this progress. With this rapid progress, it is difficult to trend and track effective PAP therapy and the associated products to learn what the best tools and methods are to obtain improved outcomes. A large database of patient information will allow analysis of the data and help to evaluate what products and methods provide the best outcomes, and standards can be developed to help the entire field of sleep medicine to improve the process of PAP therapy for the patient’s benefit.
Robert McCoy, BS, RRT, FAARC, is managing director, Valley Inspired Products Inc, Apple Valley, Minn.





