Scientists are exploring how sleep apnea phenotyping could lead to more precise care by helping to determine in advance which patients will benefit from oral appliance therapy.
By John McCormack
It is undoubtedly difficult to predict which obstructive sleep apnea (OSA) patients will find relief from their symptoms with oral appliance therapy. In most patients, we know that oral appliances may lower the apnea-hypopnea index (AHI) at least slightly. Nearly 48% of OSA patients, on average, have their AHI reduced to below five events per hour. By contrast, about a third of sleep apnea patients experience no AHI improvement whatsoever with oral appliance therapy.1
The elephant in the room, however, is that science can’t yet predict how any given patient will respond to oral appliance therapy, if at all. Now, advances in research and clinical practice are moving sleep medicine in that direction by pinpointing specific biological traits that could be used to develop phenotypes that are strongly associated with who will do well on oral appliance therapy.
“The patient says, ‘I don’t want to go and talk to my sleep doctor anymore because I am not using the [CPAP] machine and I am embarrassed.’ So, follow-up with that patient sort of gets lost. But if the sleep provider had a model that would accurately predict the likelihood of a good response with an oral appliance, then the patient could get sent directly to an oral appliance,” says Daniel Vena, PhD, an instructor in medicine at Brigham and Women’s Hospital and Harvard Medical School, and first author of a paper about predicting sleep apnea responses to oral appliance therapy using polysomnographic airflow.2
Some clinicians employ AHI as a predictor of oral appliance response, but research suggests it is not ideal.3 “In our lab, our view is it is probably a little bit more complicated than that,” Vena says.
His team developed a sleep apnea phenotyping model that calculates airflow features from routine polysomnography, and combines those metrics with age and body mass index, to predict which patients will respond favorably to oral appliance treatment responders from nonresponders with 74% accuracy.
“If you have a very, very severe collapse, then it will be harder to treat with an oral appliance,” Vena explains. Deeper respiratory events (as defined by the average drop in airflow) are associated with an airway that is more collapsible and thereby less responsive to OA. “People with shallower events were more likely to respond to oral appliance therapy,” he says.
The site of collapse is another metric incorporated into the predictive model. “If you pull the lower jaw forward, then you’re pulling the tongue out the way so you’ll likely be solving a tongue base collapse,” he says. This is in contrast to patients who exhibit palate collapse, who in general are nonresponders to oral appliance therapy. On polysomnographic recordings, Vena’s team observed that palate collapse is represented by a pinched appearance of the expiratory flow shape (caused by bulging or prolapse of the palate during expiration). Patients with more pinched expirations were less likely to respond to oral appliances.
Vena’s findings won’t be of direct use in clinical practice unless the metrics and calculations are incorporated into commercial sleep study software. Additionally, since the data was derived from a retrospective sample, more research is needed to confirm the findings, he says.
More Research Into Oral Appliance Responsiveness
New research is also suggesting that upper-airway collapsibility and loop gain predict patient response to oral appliances.4
In fact, in a randomized crossover study of 12 people with obstructive sleep apnea, these two traits explained 70% of the variance in AHI reduction. Specifically, it found that oral appliance responders had a less collapsible airway and lower loop gain compared with nonresponders.4
First author of the paper, Bradley Edwards, PhD, a Monash University associate professor and head of the sleep disorders research laboratory, as well as deputy director of the Sleep and Circadian Medicine Laboratory, says, “This work, combined with some of the newer findings, showed for the first time that understanding the physiology causing OSA provides critical information regarding which people will benefit from a particular therapy—taking the field one-step closer towards being able to deliver a personalized med approach.”
But “having simple ways to assess the underlying physiology causing OSA” continues to be a barrier to predicting oral appliance response, Edwards says. “Much progress has been made in this domain, but there are still a lot of questions we need answers to before this becomes prime time.”
Most predictive models focus on AHI reduction and not on other outcomes of oral appliance therapy, he also notes, such as whether the patient is likely to adhere to the device or if it will improve symptoms such as excessive daytime sleepiness.
Real World Attempts to Predict Oral Appliance Response
Reza Radmand, DMD, DABDSM, FAAOM, of Advanced Dental Sleep Medicine, does ask patients who use oral appliances about their symptom improvement, but “the response is based on their subjective observations and that is really not good enough,” he says.
Radmand, a coauthor with Vena on the polysomnographic airflow paper2 and a research collaborator in sleep medicine at Brigham and Women’s Hospital, says there are some objective ways to predict whether an OSA patient is likely to respond to oral appliances. But each method has its pros and cons.
Drug-induced sleep endoscopy (DISE), a procedure done under anesthesia, provides a “great deal of anatomical and physiological observations in a sleep patient,” Radmand says, and therapeutic modalities such as mechanical movement of the lower jaw or external tongue stimulation can be tried to evaluate efficacy.
But DISE is costly, requires a special facility and expert staff, and comes with the risks commonly associated with anesthesia.
What’s more, while DISE can determine if a patient will positively respond to OA therapy, its findings don’t necessarily help the sleep practitioner build a custom device.
“The dentist essentially starts over and may or may not achieve the same results as that achieved during DISE,” says Dan Levendowski, MBA, president of Advanced Brain Monitoring, marketers of sleep diagnostic and therapy devices.
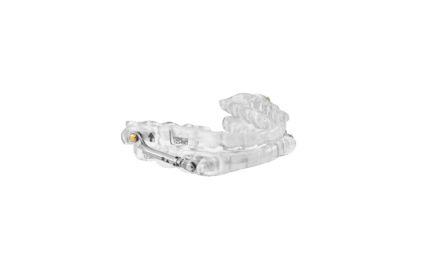
Trial oral appliances—transitional devices that provide immediate therapy for the patient and can act as a bridge to long-term custom oral appliances—can also provide some insight. For example, the odds of an Advanced Brain Monitoring Apnea Guard trial oral appliance identifying positive outcomes in patients treated with a custom oral appliance was 3.4, according to one study, and the odds of the trial oral appliance identifying patients who would achieve an AHI of less than 10 with the custom oral appliance was 4.0.5
But Radmand notes, patients have been dissuaded from oral appliance therapy after using a trial oral appliance that wasn’t as comfortable or efficacious as a custom device would have been.
In other countries, sleep clinicians have found success combining DISE and trial oral appliances to predict response in sleep apnea patients, Levendowski says. “In Europe, [ear-nose and throat physicians] are now using the Apnea Guard during DISE to more systematically adjust the airway during the procedure, and it enables their DISE conclusions to be transferred directly to the custom [oral appliance] by the dentist,” he says.
Multi-therapy trials—in which patients undergo multiple consecutive nights of sleep studies at home, trialing a different therapy each night—can also help determine the most effective therapy, whether oral appliance, positional device, or CPAP. However, this approach is costly and time-consuming.
“We’ve conducted a number of studies whereby multi-night home sleep tests (HSTs) were used to identify treatment response and guide therapy decisions,” Levendowski says. “From these studies we’ve learned, for example, that it’s unlikely that oral appliance therapy will be optimized unless vertical mouth opening is effectively managed in patients with extended supine sleep time.”6
Levendowski has also developed software—which is available at no cost (at https://tinyurl.com/bdzdnx9z)—to determine which therapy is the best fit for a given patient. “To help clinicians formulate a treatment plan based on multi-night HST results, we’ve developed software…that applies the necessary computations, summarizes the results, and highlights therapy considerations when applicable,” he says.
Why Prediction Matters
An abstract presented at the American Academy of Dental Sleep Medicine 2021 meeting revealed that 88% of sleep physicians find the “unpredictable, variable” performance of oral appliance therapy as a barrier to prescribing it for sleep apnea patients. But abstract author Len Liptak, CEO of oral appliance maker ProSomnus Sleep Technologies, says that sleep physicians also indicated a strong willingness to prescribe such treatment more frequently if oral appliance therapy could demonstrate more predictable, efficacious outcomes.7
In Liptak’s view: “Although more research is needed, the best available evidence suggests that the most simplistic, predictable, and efficacious approach would be to treat mild and moderate obstructive sleep apnea patients with precision-style oral appliances, and then apply phenotyping techniques to the severe obstructive sleep apnea patients and the mild and moderate sleep apnea patients who do not respond to precision-style oral appliance therapy devices.”
Accurately predicting oral appliance response would be a boon for patients. As dentist and researcher Radmand notes, “The ability to identify predictive patient response to oral appliance therapy will reduce treatment cost, shorten the time to reach optimal therapeutic goals, and could reduce obstructive sleep apnea-related comorbidities.”
John McCormack has been a healthcare writer for more than 20 years. This is his first article for Sleep Review.
References
1. Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10(2):215-27.
2.Vena D, Azarbarzin A, Marques M, et al. Predicting sleep apnea responses to oral appliance therapy using polysomnographic airflow. Sleep. 2020;43(7):zsaa004.
3. Okuno K, Pliska BT, Hamoda M, et al. Prediction of oral appliance treatment outcomes in obstructive sleep apnea: A systematic review. Sleep Med Rev. 2016 Dec;30:25-33.
4. Edwards BA, Andara C, Landry S, et al. Upper-airway collapsibility and loop gain predict the response to oral appliance therapy in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 2016;194(11):1413-22.
5. Morgan T, Munafo D, Clark SJ, et al. Comparison of efficacy from a custom and trial oral appliance. 2019 AADSM Meeting Abstract.
6. Levendowski D, Clark SJ, Odom W, et al. The influence of sex, tongue size and sleeping position on oral appliance therapy outcomes. JDSM. 10 Apr 2020;7.2: Abstract #021.
7. Liptak L. What do we know about sleep medicine physicians? JDSM. 2021 AADSM Virtual Annual Meeting Abstracts: Abstract #12.
Photo 9142488 © Petesaloutos | Dreamstime.com