A new report by the Agency for Healthcare Research and Quality (AHRQ) finds that, among treatments for obstructive sleep apnea (OSA), continuous positive airway pressure (CPAP) machines and a mandibular advancement device (MAD) worn at night are effective, with CPAP being backed by the strongest evidence. Weight loss and surgery may also be effective, although evidence behind these treatments is not as strong, according to the report, titled “Comparative Effectiveness Review of the Diagnosis and Treatment of Obstructive Sleep Apnea in Adults,” conducted by the Tufts Medical Center Evidence-based Practice Center for AHRQ’s Effective Health Care Program.
The report—a review of 234 clinical studies published through 2010—finds that a CPAP machine is highly effective at improving sleep and related symptoms of OSA by improving airflow. However, the report also finds that use of a CPAP machine includes possible side effects—such as feeling trapped, dry nose and mouth, nosebleeds, and chest discomfort—that may lead patients to abandon treatment. Additionally, the report notes that the CPAP machine is effective only if it is used every night.
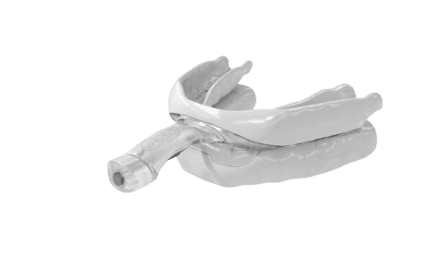
The report finds MADs are also effective but have possible side effects of their own, including potentially loose or damaged teeth.
The report further finds that there is not enough evidence to determine if surgery to clear airway blockage, the third major treatment for OSA, is more or less effective than nonsurgical treatments. Other treatments—including weight loss programs and medication—were also examined, but the evidence was insufficient to draw conclusions about these treatments, according to the report.
Additionally, the report looks at the evidence supporting the effectiveness of portable monitoring to diagnose OSA. The report concludes, “The strength of evidence is low that Type II monitors are accurate to diagnose OSA (as defined by PSG), but have a wide and variable bias in estimating the actual AHI.” Meanwhile, the report finds, “The strength of evidence is moderate that Type III and IV monitors are generally accurate to diagnose OSA (as defined by PSG), but have a wide and variable bias in estimating the actual AHI.” The report notes that evidence is insufficient to adequately compare specific monitors to each other.
In addition to the report, the AHRQ has also made a series of companion comparison guides available for consumers and clinicians that summarize the report’s findings. The consumer guide defines sleep apnea for patients and their families, summarizes treatment options, and offers a list of questions for patients to discuss with their doctor. The clinician guide, meanwhile, covers the same topics as the consumer guide, while also providing “confidence ratings” for existing scientific evidence and offering a “clinical bottom line” to give clinicians tools to discuss treatment options with the patients.